1. Shrivastava A, Johnston M, Terpstra K, Stitt L, Shah N. Atypical antipsychotics usage in long-term follow-up of first episode schizophrenia. Indian J Psychiatry. 2012 Jul;54(3):248-52. doi: 10.4103/0019-5545.102425. PMID: 23226849; PMCID: PMC3512362. [cited 2022 July 22]
2. Insel T, “Antipsychotics: Taking the Long View” Open Excellence, (Thomas Insel, former NIMH Director) 2013 Aug, National Institute for Mental Health [cited 2022 July 22]
3. Klawans HL, Tanner CM, Barr A. The reversibility of “permanent” tardive dyskinesia. Clin Neuropharmacol. 1984;7(2):153-9. doi: 10.1097/00002826-198406000-00006. PMID: 6145520. [cited 2022 July 22]
4. Cornett et al., “Medicine-Induced Tardive Dyskinesia: A Review and Update” National Institute for Mental Health [cited 2022 July 22]
5. Crowley et al., “Brain Levels of the Neurotoxic Pyridinium Metabolite HPP+ and Extrapyramidal Symptoms in Haloperidol-Treated Mice.” Neurotoxicology 2013 Dec., PMID24107597 [cited 2022 July 22]
6. FDA drug label Invega (paliperidone} Extended Release Tablets, approved 2006 [cited 2022 July 22]
7. NAMI authors, “Paliperidone (Invega) [published online Feb 2020] [cited 2022 July 22]
8. Oxford References, “Ulysses contract” [published online 2022] [cited 2022 July 22]
9. Keks N, Schwartz D, Hope J. Stopping and switching antipsychotic drugs. Aust Prescr. 2019;42(5):152-157. doi:10.18773/austprescr.2019.052 [cited 2022 July 22]
10. Hedges DW, Woon FL, Hoopes SP. Caffeine-induced psychosis. CNS Spectr. 2009 Mar;14(3):127-9. doi: 10.1017/s1092852900020101. PMID: 19407709. [cited 2022 July 22]
11. Wang HR, Woo YS, Bahk WM. Caffeine-induced psychiatric manifestations: a review. Int Clin Psychopharmacol. 2015 Jul;30(4):179-82. doi: 10.1097/YIC.0000000000000076. PMID: 25856116. [cited 2022 July 22]
12. NIDA. 2020, May 28. Is there a link between marijuana use and psychiatric disorders? [cited 2022 July 22]
13. Henquet C, Di Forti M, Morrison P, Kuepper R, Murray RM. Gene-environment interplay between cannabis and psychosis. Schizophr Bull. 2008;34(6):1111-1121. doi:10.1093/schbul/sbn108. [cited 2022 July 22]
14. Nesvåg R, Frigessi A, Jönsson EG, Agartz I. Effects of alcohol consumption and antipsychotic medication on brain morphology in schizophrenia. Schizophr Res. 2007 Feb;90(1-3):52-61. doi: 10.1016/j.schres.2006.11.008. Epub 2007 Jan 10. PMID: 17218084. [cited 2022 July 22]
15. Wen Q, Chklovskii DB. Segregation of the brain into gray and white matter: a design minimizing conduction delays. PLoS Comput Biol. 2005;1(7):e78. doi:10.1371/journal.pcbi.0010078 [cited 2022 July 22]
16. Sahoo S, Mehra A, Grover S. Acute Hyperglycemia Associated with Psychotic Symptoms in a Patient with Type 1 Diabetes Mellitus: A Case Report. Innov Clin Neurosci. 2016;13(11-12):25-27. Published 2016 Dec 1. [cited 2022 July 22]
17. Hormone Health Network Non-Diabetic Hypoglycemia EDITOR(S): Prof. Margaret Eckert-Norton, PHD, FNP-BC, CDE, Ramon Martinez, M.D., Susan Kirk, M.D. LAST UPDATED: July 2020. [cited 2022 July 22]
18. Sharma A, Madaan V, Petty FD. Exercise for mental health. Prim Care Companion J Clin Psychiatry. 2006;8(2):106. doi:10.4088/pcc.v08n0208a [cited 2022 July 22]
19. Callaghan P. Exercise: a neglected intervention in mental health care? J Psychiatr Ment Health Nurs. 2004 Aug;11(4):476-83. doi: 10.1111/j.1365-2850.2004.00751.x. PMID: 15255923. [cited 2022 July 22]
20. Janssen drug information Invega “How to take Invega” [published online 2019] [cited 2022 July 22]
21. Andrade C. Delayed drug interactions in psychiatry: armodafinil and risperidone as a potential case in point. J Clin Psychiatry. 2015 Dec;76(12):1633-4. doi: 10.4088/JCP.15f10514. PMID: 26717524. [cited 2022 July 22]
22. Brandt L, Bschor T, Henssler J, et al. Antipsychotic Withdrawal Symptoms: A Systematic Review and Meta-Analysis. Front Psychiatry. 2020;11:569912. Published 2020 Sep 29. doi:10.3389/fpsyt.2020.569912 [cited 2022 July 22]
23. Chemerinski E, Ho BC, Flaum M, Arndt S, Fleming F, Andreasen NC. Insomnia as a predictor for symptom worsening following antipsychotic withdrawal in schizophrenia. Compr Psychiatry. 2002 Sep-Oct;43(5):393-6. doi: 10.1053/comp.2002.34627. PMID: 12216015. [cited 2022 July 22]
24. Horowitz MA, Jauhar S, Natesan S, Murray RM, Taylor D. A Method for Tapering Antipsychotic Treatment That May Minimize the Risk of Relapse. Schizophr Bull. 2021 Mar 23:sbab017. doi: 10.1093/schbul/sbab017. Epub ahead of print. PMID: 33754644. [cited 2022 July 22]
25. Aucoin M, LaChance L, Clouthier SN, Cooley K. Dietary modification in the treatment of schizophrenia spectrum disorders: A systematic review. World J Psychiatry. 2020 Aug 19;10(8):187-201. doi: 10.5498/wjp.v10.i8.187. PMID: 32874956; PMCID: PMC7439299. [cited 2022 July 22]
26. Morrison AK. Cognitive behavior therapy for people with schizophrenia. Psychiatry (Edgmont). 2009;6(12):32-39. [cited 2022 July 22]
27. Barnes TR, Paton C. Antipsychotic polypharmacy in schizophrenia: benefits and risks. CNS Drugs. 2011 May;25(5):383-99. doi: 10.2165/11587810-000000000-00000. PMID: 21476610. [cited 2022 July 22]
28. Borlido C, Remington G, Graff-Guerrero A, Arenovich T, Hazra M, Wong A, Daskalakis ZJ, Mamo DC. Switching from 2 antipsychotics to 1 antipsychotic in schizophrenia: a randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2016 Jan;77(1):e14-20. doi: 10.4088/JCP.14m09321. PMID: 26845273. [cited 2022 July 22]
29. Loughlin AM, Lin N, Abler V, Carroll B. Tardive dyskinesia among patients using antipsychotic medications in customary clinical care in the United States. PLoS One. 2019 Jun 4;14(6):e0216044. doi: 10.1371/journal.pone.0216044. PMID: 31163035; PMCID: PMC6548364.[cited 2022 July 22]
30. Jeste D V, et al, “Tardive Dyskinesia-Reversible and Permanent” JAMA May 1979 [cited 2022 July 22]
31. Yin J, Barr AM, Ramos-Miguel A, Procyshyn RM. Antipsychotic Induced Dopamine Supersensitivity Psychosis: A Comprehensive Review. Curr Neuropharmacol. 2017;15(1):174-183. doi:10.2174/1570159×14666160606093602 [cited 2022 July 22]
32. MacNeil RR, Müller DJ. Genetics of Common Antipsychotic-Induced Adverse Effects. Mol Neuropsychiatry. 2016;2(2):61-78. doi:10.1159/000445802 [cited 2022 July 22]

 The generic name for Invega is paliperidone and is also available under other brand names, in a time-release or injectable form, which may introduce some added complications for Invega tapering. It is one of the atypical antipsychotic medications that have become widely used for treating schizophrenia, schizoaffective and bipolar-related mania, episodes of psychosis, and other critical conditions.
The generic name for Invega is paliperidone and is also available under other brand names, in a time-release or injectable form, which may introduce some added complications for Invega tapering. It is one of the atypical antipsychotic medications that have become widely used for treating schizophrenia, schizoaffective and bipolar-related mania, episodes of psychosis, and other critical conditions.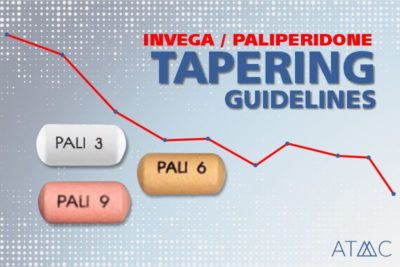 Aim to begin your taper when you are stable, sleeping and eating well, and not experiencing psychotic or other major symptoms — except for life-threatening medical reasons such as NMS. In all cases, medical oversight should guide the starting and stopping of antipsychotic medications.6,7
Aim to begin your taper when you are stable, sleeping and eating well, and not experiencing psychotic or other major symptoms — except for life-threatening medical reasons such as NMS. In all cases, medical oversight should guide the starting and stopping of antipsychotic medications.6,7 Antipsychotic drugs are most concerning because they are noted for causing significant side effects, especially after long-term usage. Tardive dyskinesia, for example, has been observed in 16-50% of patients on antipsychotic medications, a number according to research by Loughlin et al published in the 2019 Journal of PLoS One is likely underestimated.29 Other adverse effects include elevated blood sugar levels, weight gain, high cholesterol, Parkinson’s disease or Parkinson’s-like conditions, dystonia, cogwheel rigidity (rigid limbs/muscles), and akathisias as mentioned on Invega’s label insert. Also of concern, antipsychotics may precipitate or aggravate certain heart problems such as cardiac arrest, stroke, and long QT syndrome.6 This type of drug can cause many other potential side effects that can negatively impact a person’s health and reduce their quality of life. When the initial crisis of a psychotic episode or other mental health event has passed, a person may consider Invega tapering and the use of Invega alternatives to avoid these types of risks.
Antipsychotic drugs are most concerning because they are noted for causing significant side effects, especially after long-term usage. Tardive dyskinesia, for example, has been observed in 16-50% of patients on antipsychotic medications, a number according to research by Loughlin et al published in the 2019 Journal of PLoS One is likely underestimated.29 Other adverse effects include elevated blood sugar levels, weight gain, high cholesterol, Parkinson’s disease or Parkinson’s-like conditions, dystonia, cogwheel rigidity (rigid limbs/muscles), and akathisias as mentioned on Invega’s label insert. Also of concern, antipsychotics may precipitate or aggravate certain heart problems such as cardiac arrest, stroke, and long QT syndrome.6 This type of drug can cause many other potential side effects that can negatively impact a person’s health and reduce their quality of life. When the initial crisis of a psychotic episode or other mental health event has passed, a person may consider Invega tapering and the use of Invega alternatives to avoid these types of risks. Antipsychotics can affect several types of neurotransmitters and their receptors. Regarding dopamine, for example, the drug is thought to create hypersensitive dopamine receptors along the CNS pathways while concurrently setting up a chronic dopamine blockade that is also medication-induced. This can cause a cascade of other responses including oxidative stress and cell death.31
Antipsychotics can affect several types of neurotransmitters and their receptors. Regarding dopamine, for example, the drug is thought to create hypersensitive dopamine receptors along the CNS pathways while concurrently setting up a chronic dopamine blockade that is also medication-induced. This can cause a cascade of other responses including oxidative stress and cell death.31